India has now become the Diabetes capital of the world. At present, approximately 15% of Indians have Diabetes and another 25% are Pre-Diabetic.
The numbers have tripled since the 1980s and are projected to double in the next decade alone. However, scarier still is that there are about 1 million Diabetes-related deaths in the country every year.
These numbers are growing unabated due to a lack of knowledge about Diabetes. Most Diabetes patients have a very non-serious approach to Diabetes despite it being the root of many other diseases.
Many of us think of Diabetes as simply a “high blood sugar’’ problem that we must keep under “control” by avoiding sugar and/or taking insulin medication. However, high blood sugar is merely an effect of Diabetes and not the cause.
Many others do not know the type of Diabetes they suffer from or how the various types of Diabetes differ in cause, effect, and treatment. So let’s explain some common queries around Diabetes and shed some light on the various types.
WHAT IS DIABETES?
Simply put, Diabetes is a problem caused by unregulated insulin levels in the blood, which results in elevated blood sugar levels.
Insulin is a hormone produced in the pancreas. Besides its other functions, insulin regulates our blood glucose level and plays an essential role in metabolism (digestion of food and energy production).
In digestion, carbs are broken down into glucose before they enter the bloodstream. This glucose is absorbed into our cells with the help of insulin to produce energy. In short, insulin is like a key that opens the doors to the cells for the glucose to enter.
If more glucose is in the bloodstream, the pancreas produces more insulin and releases it into the bloodstream. After the glucose enters the cells, the blood glucose level returns to normal. In a healthy person, these functions allow blood glucose and insulin levels to remain normal. But in a diabetic person, either the pancreas doesn’t produce enough insulin (Type 1 diabetes), the cells are insulin resistant (Type 2 diabetes), or both.
As a result, the blood glucose does not pass into the cells, thus causing high blood sugar, apart from other symptoms.
HOW DOES DIABETES DEVELOP?
When we have a highly refined carb-rich diet, we produce more insulin and excess sugar in our blood. The pancreas produces more insulin to pass this blood glucose into our cells. If this continues for a long time, the cells start becoming resistant to the effect of insulin. Since the blood sugars are still not passing into the cells, the pancreas produces even more insulin, and the vicious cycle is completed. This phenomenon is called insulin resistance.
There can be many root causes of insulin resistance, such as ultra-processed foods, inflammation, infections, stress, toxic exposure, lack of sleep, dehydrated water etc. But the bottom line is that there needs to be more than ingesting insulin exogenously to fix the underlying problem.
If we eat carbs, they will still be digested and converted into blood sugar, and our pancreas will produce the required amount of insulin to help it pass into the cells. However, the transfer of sugars into the cells will not happen if the cells are insulin resistant. So when we take insulin on top of it, we have high blood sugar and high insulin. Unfortunately, due to this broken process, when we take insulin over some time, it puts an excess load on the pancreas, which leads to pancreatic and kidney degeneration.
It is noteworthy here that insulin resistance starts many years before a person is diagnosed with Diabetes or even Pre-diabetes. Some of the early signs of increased insulin levels are an increase in appetite, weight gain around the belly, darkening of the skin around the neck and underarms, skin tags, inability to lose weight, brain fog, inability to skip a meal, fatigue and tiredness, post-meal fatigue, inflammation and oxidative stress etc.
WHAT ARE THE TYPES OF DIABETES?
Predominantly, there are five kinds of Diabetes that we will discuss from now on.
Type 1 Diabetes
In the case of Type-1 Diabetes, the Pancreas produce little or no insulin. This happens when the immune system (which usually protects our body from infections by fighting bacteria, viruses etc.) attacks and destroys our own cells that make insulin.
This usually occurs in childhood and teenagers but can happen at any age. Type-1 people with Diabetes are dependent on regular insulin injections for the management of Diabetes.
Type 2 Diabetes
90-95% of all Diabetes cases are of Type-2. Diabetes is typically characterized by high blood sugar and high to normal insulin levels. In a person without Diabetes, the appropriate insulin levels would rapidly reduce the blood sugar to normal.
But in Type-2 Diabetes, the cells become insulin resistant, making blood sugar hard to control with insulin or any other medication.
Type 1.5 Diabetes
This is a lesser-known type of Diabetes that falls between Type-1 and Type-2 and is also called LADA or Latent Autoimmune Diabetes in Adults. Like in Type-1, the Pancreas doesn’t produce enough insulin, and the body becomes dependent on exogenous insulin for its functioning.
However, unlike Type-1, the damage to the Pancreas is not very serious and can be stopped with proper care and treatment. Thus, the dependency on insulin can be minimized. With specific lifestyle changes, this type of Diabetes can also be reversed, just like Type-2.
Pre-diabetes
This is an early stage of insulin resistance where the blood sugar is elevated above average but not high enough to be called Type-2 Diabetes. This is like an alarm bell requiring us to start the reversal process before things worsen. You are not in the safety zone anymore. So many complications start to happen at this stage.
Gestational Diabetes
Gestation Diabetes or pregnancy diabetes is typically diagnosed between the 24th and 28th week of pregnancy and is caused due to deficiency of functional vitamin B6. Impaired Tryptophan metabolism with increased production of Xanthurenic acid and Kynurenic acid antagonizes the insulin. This triggers insulin resistance.
Gestational Diabetes symptoms may include frequent urination, frequent thirst, dryness of the mouth, tiredness, blurred vision and genital itching or thrush.
Usually, insulin shots are prescribed to bring the sugars down to normalcy. However, Gestational Diabetes treatment with insulin can cause macrosomia in the fetus and maternal and fetal complications during delivery.
The impact may even continue till after the postnatal period. So alternatively, 100 mg/day of Vitamin B6 supplements can be prescribed for 2-3 weeks to correct the Tryptophan metabolism and reverse Gestational Diabetes.
In addition, patients not responding to the B6 supplementation can be given personalized dietary protocols based on low insulin dietary regimen.
TYPE-1 DIABETES VS TYPE-2 DIABETES
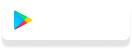
Now that we understand the basics, we can delve deeper into the differences between Type-1 and Type-2 Diabetes. Although both Type-1 and Type-2 Diabetes are typified by high blood sugar, they are entirely different in their pathophysiology.
What is Type-1 Diabetes?
Type-1 Diabetes is a disorder of insulin insufficiency, which means that the pancreas cannot produce enough insulin, so blood sugar cannot be absorbed into the cells.
The low insulin production in the pancreas is attributed to the autoimmune destruction of the beta cells or the immune system’s self-destruction of the insulin-producing cells in the pancreas. It usually occurs in childhood and teenagers but can occur later in life too.
What is Type-2 Diabetes?
Type-2 Diabetes is a disorder of insulin inefficiency caused by insulin resistance driven by high insulin diet due to ultra-processed foods. Insulin resistance is when insulin production is normal or high, but the cells stop responding to insulin due to underlying lipotoxicity.
High insulin combined with refined carbs and oils intake causes lipotoxicity, simply the deposition of fats in non-adipose organs or organs that are not designed to store fats, such as the liver, pancreas and viscera.
Release of excess free fatty acids from the viscera also causes fatty liver, inhibiting glucose uptake by the muscle cells. Type-2 Diabetes usually occurs in middle age.
However, lately, there has been an increase in cases of Type-2 Diabetes in the young adult and pediatric age groups as well. For example, 1/3rd of all Diabetes cases in the pediatric age group are Type-2 nowadays.
However, it is often mistaken for Type-1 and treated incorrectly with insulin ingestion. Therefore, measuring the C-peptide level (a measure of insulin reserve or functional beta cell volume) is mandatory before starting insulin therapy on any patient.
What is the difference between Type-1 Diabetes and Type-2 Diabetes?
From the above, it can be concluded that the most significant difference between Type-1 Diabetes Vs Type-2 Diabetes is that Type-1 Diabetes is a disorder of insulin insufficiency (the pancreas does not produce enough insulin to be able to absorb the blood sugars into the cells).
Whereas Type-2 Diabetes is a disorder of insulin inefficiency (the pancreas is producing sufficient insulin to be able to absorb the blood sugars into the cells, but the cells have become insulin resistant. And hence, they do not allow the absorption to happen).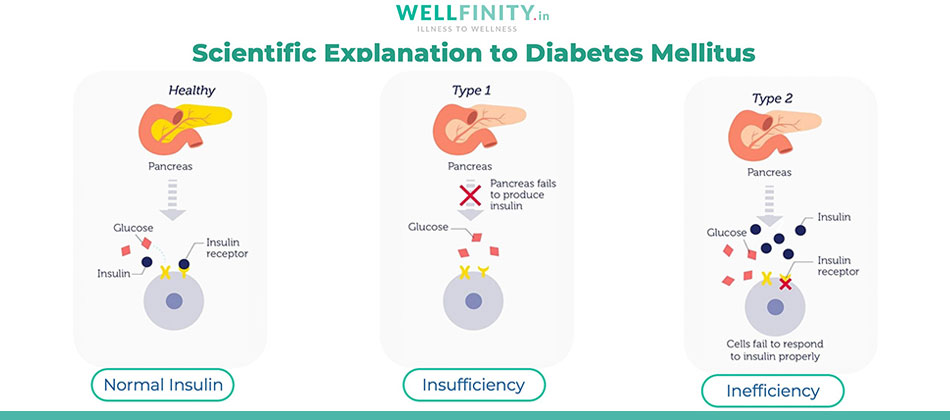
What are the symptoms of Type-1 Diabetes and Type-2 Diabetes?
Since both Type-1 and Type-2 Diabetes are typified by high blood sugar, many of the symptoms of Type 1 vs Type-2 Diabetes are more or less the same. However, Type-1 Diabetes symptoms appear more quickly than Type-2 Diabetes symptoms. Some of the common symptoms diabetics experience are as follows:
- Difficulty focusing
- Fatigue
- Poor sleep
- Blurred vision
- Increased thirst and dry mouth
- Slow-healing sores or frequent infections
- Increased hunger/weight gain
- Neuropathy (numbness, tingling in feet and hands)
- Increased urination
- Frequent vaginal or urinary infections
- Erectile dysfunction
In the case of Type-1 Diabetes, patients may have some other symptoms as well. These are as follows:
- Nausea
- Vomiting
- Abdominal pain
- Recurring yeast infection or Candidiasis
Since Type-1 Diabetes frequently occurs in children, the symptoms can be challenging to notice. We would need to watch out for symptoms like:
- Bedwetting
- Changes in appetite
- Changes in behaviour more severe than regular mood changes
- Diaper rashes that won’t go away
What are the treatment options for Type-1 Diabetes and Type-2 Diabetes?
Unlike the symptoms, the treatment for Diabetes Mellitus Type-1 Vs Type-2 is entirely different.
Type-1 Diabetes was considered a death sentence 100 years ago until the discovery of insulin proved to be a lifesaver. There is no easy treatment for the reversal of Type-1 diabetes except if it is in an early phase, in which case gluten and A1 dairy have to be eliminated from the diet.
Otherwise, treatment of Type-1 diabetes usually entails keeping blood sugar levels under control using exogenous insulin. Type-1 people with diabetes can thus lead a near-normal life with insulin therapy.
People looking for miraculous cures for Type-1 diabetes are often misled into alternative therapies and eventually end up with life-threatening complications like Diabetes Ketoacidosis (DKA) when they skip insulin for a few days or weeks. People with Type-1 diabetes have no insulin production, and it needs to be supplemented lifelong.
However, it is essential to remember that the appropriate insulin dose is administered. High doses of insulin can cause dual diabetes – a combination of Type-1 and Type-2 diabetes in which the patient may not be able to produce endogenous insulin. At the same time, he may develop insulin resistance. In this case, it becomes difficult to manage.
However, there is a possibility that the mechanism of the disorder can be controlled with a change in habits, especially dietary and exercise routines. If healthy habits are maintained, the diseases pose less of a threat.
For example, the patient may be insulin dependent if the pancreatic beta cells are destroyed (as with autoimmune Type-1 disease).
Still, the need for insulin will decrease as the patient develops increased control of blood sugar metabolism. In the long term, the reduced dosage of exogenous insulin will prevent side effects due to the chronic use of synthetic insulin.
In addition, the improved natural metabolism will provide impossible health benefits with synthetic insulin.
In the case of Type-2 Diabetes Mellitus, the patient already has insulin resistance. Giving him exogenous insulin will increase insulin resistance. The increased insulin resistance will be managed with higher doses of exogenous insulin, thus completing a vicious cycle.
Eventually, the patient on insulin therapy will put on weight over time, and there is no downtrend, which makes his life difficult.
Moreover, insulin resistance occurs due to mitochondria dysfunction. Mitochondria is the engine that drives our cells. Due to the impact of our external and internal environment, the quantity and quality of mitochondria in our cells deteriorate. This directly impacts the cell’s ability to absorb blood sugars. Thus, there is more unabsorbed sugar in our blood.
The scientific and sustainable solution for Type-2 Diabetes is to switch from a high-insulin diet to a low-insulin diet as it can reverse Type-2 Diabetes. When insulin levels are low, excess energy is wasted by burning fats (particularly the visceral fats, which are metabolically active) and hence used up preferentially when compared to subcutaneous fat.
Low insulin diet consists of complex carbs, saturated fats, animal-sourced foods, and MUFA (monounsaturated Fatty acids) with the right combinations at the right time. A high insulin diet that causes insulin resistance in the first place includes highly refined carbohydrates, refined oils, gluten, dairy, and excess sugars that must be eliminated. Fasting helps in reducing Fatty liver and, thence, insulin resistance.
Since Type-2 Diabetes is a metabolic problem, the mitochondria function should also be restored. This can be possible by correcting circadian mismatch or misalignment, consuming structured water, eating a balanced diet, reducing consumption of heavy metals, and supplementing for the deficit of minerals and vitamins essential for mitochondria replacement and repair.
There is a misconception that Type-2 Diabetes Mellitus can run in the family due to genetics. The fact is, Type-2 Diabetes is a non-communicable disease. It does not spread from person to person, even through genes. Instead, it happens because of Epigenetics – the impact of our internal and external environment on our genes, including unhealthy food and lifestyle factors.
By switching to a healthy diet and adopting a healthy lifestyle, we can reverse Type-2 Diabetes effectively and sustainably. We are not victims of our genes but masters of them.
The concept of “Type-2 is a chronic progressive disease” is outdated science, and hopefully, the reversal of Type-2 Diabetes should become the new norm in the coming years.
What are the risk factors for Type-1 and Type-2 Diabetes?
The primary complications of Type-1 Diabetes Mellitus vs Type-2 are sub-divided as follows:
- Microvascular complications and
- Macrovascular complications
Microvascular complications are complications of the small vessels, such as Neuropathy (neuropathic pain in the extremities), retinopathy (loss of vision) and nephropathy (decreased renal function).
On the other hand, macrovascular complications lead to buildup and ectopic deposits of fats, cholesterol and other substances in and on the artery walls and large vessels. In addition, they can lead to strokes, cardiovascular and heart complications and peripheral vascular disease (e.g. gangrene of the foot).
Both microvascular and macrovascular complications are caused by insulin toxicity, which remodels or changes the vasculature. Microvascular complications are often exacerbated when glucose levels (the sorbitol pathway which converts glucose into sorbitol and fructose) are high. This increases the osmotic and oxidative stress in the affected organ.
Summary
In summation, Type-1 and Type-2 Diabetes are both typified by high blood sugars and may have similar symptoms. However, Type-1 Diabetes vs Type-2 Diabetes can be differentiated by their cause and treatment.
In Type-1 Diabetes, the blood sugar is high due to low production of insulin in the pancreas, and thus Type-1 Diabetes treatment involves ingesting the right amount of exogenous insulin.
However, over some time, insulin dependency can be reduced. On the other hand, in Type-2 Diabetes, the pancreas produces enough insulin to absorb the blood sugars into the cells, but the cells are insulin resistant and do not allow the absorption.
Hence, Type-2 Diabetes treatment should involve lifestyle and dietary changes to reverse the disease. Type-1 Diabetes may not be completely reversible in all cases, but it can be stopped if detected early.