45 year old Kumar woke up each morning feeling drained. He struggled to focus at work, and noticed a decline in his energy and drive. Despite a healthy diet and regular exercise, he felt something was off. His motivation was waning, and his once vibrant energy seemed a distant memory.
If Kumar’s condition sounds familiar, then you too might be experiencing symptoms of hormonal imbalance – particularly low testosterone. But the good news is, that bio-identical hormone replacement therapy (BHRT) and testosterone replacement therapy (TRT) can effectively restore energy and enhance your quality of life.
This blog explains the science, benefits, and holistic methods of hormone therapy, using functional medicine insights to help you understand how these treatments can address hormonal imbalances and support long-term health.
What Are BHRT and TRT?
Hormone therapy aims to restore balance to the body’s hormonal systems – which regulate essential functions like energy, mood, and physical performance. Bioidentical hormone replacement therapy (BHRT) uses hormones identical in molecular structure to those naturally produced by the body. They are derived from plant-based sources such as soy or yams. These hormones are chemically identical to those produced by the human body such as testosterone, estrogen, progesterone, and DHEA. Thus, BHRT is a natural alternative to synthetic hormones and can be used to address a range of hormonal imbalances in both men and women, particularly during menopause, perimenopause, or andropause (male menopause).
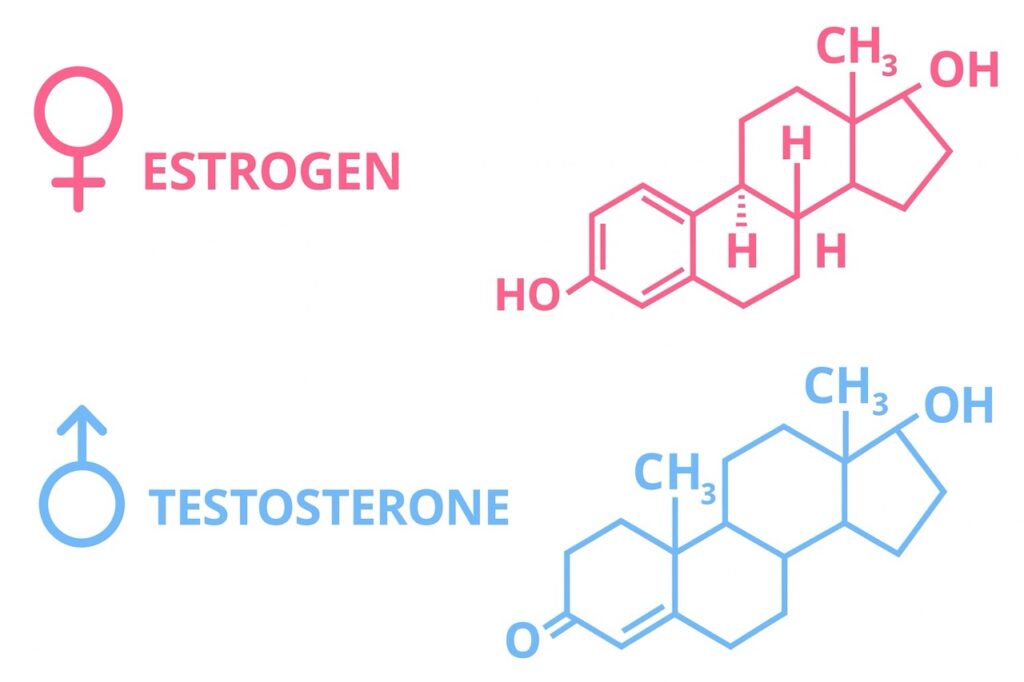
Testosterone replacement therapy (TRT), a subset of BHRT, specifically focuses on restoring testosterone levels in individuals with clinically diagnosed low testosterone – a condition known as hypogonadism. While primarily used for aging men, TRT can also benefit women in cases of low libido or energy. Testosterone plays a critical role in muscle mass, bone density, libido, and mental clarity. Both BHRT and TRT are usually custom-compounded doses tailored to individual needs and offer a personalized approach to hormone optimization.
Symptoms of Hormonal Imbalance and Low Testosterone
Hormonal imbalances manifest in various ways, significantly impacting quality of life.
For men, low testosterone can lead to persistent fatigue, reduced energy, and diminished stamina, making daily tasks feel overwhelming. Sexual health is often affected, with symptoms like decreased libido and erectile dysfunction. Physical changes include loss of muscle mass, increased body fat (particularly visceral fat), and reduced strength. Mentally, men may experience mood swings, depression, irritability, or anxiety, alongside cognitive challenges such as brain fog, poor concentration, or memory decline. Over time, low testosterone increases the risk of osteoporosis and cardiovascular issues, underscoring the need for early intervention.
Women undergoing hormonal changes, particularly during menopause or perimenopause, may experience hot flashes, night sweats, and vaginal dryness, which can disrupt daily life. Irregular periods, mood swings, low libido, fatigue, and weight gain are also common. These symptoms, while often associated with aging, are not inevitable. Recognizing them early allows individuals to seek treatment and regain control of their health.
Causes of Testosterone Deficiency
Testosterone deficiency can arise from multiple factors, both natural and environmental. Aging is a primary driver, with testosterone levels declining steadily by 1-2% per year after age 30, contributing to andropause in men. However, lifestyle factors play a significant role. Poor inflammatory diet, obesity, lack of quality sleep and exercise, alcohol consumption, poor live function, and chronic stress can suppress testosterone production. Inadequate sleep (less than 7–9 hours per night) disrupts hormone synthesis. While chronic stress elevates cortisol, a hormone that inhibits testosterone.
Environmental factors, such as exposure to endocrine disruptors like bisphenol A (BPA) found in plastics or pesticides, and heavy metal toxicity (for e.g. cadmium, lead, arsenic) can interfere with hormone production. Medical conditions also contribute, including primary hypogonadism (testicular failure), secondary hypogonadism (pituitary or hypothalamic dysfunction), and chronic illnesses like diabetes, metabolic syndrome, autoimmune conditions or cardiovascular disease.
The functional medicine perspective emphasizes additional root causes, such as poor gut health, which impairs nutrient absorption, and systemic inflammation, which disrupts hormonal balance. Identifying these underlying factors is crucial for effective treatment.
Diagnosing Hormonal Imbalances
Accurate diagnosis is the foundation of effective hormone therapy. Comprehensive blood testing is used to measure total and free testosterone, sex hormone-binding globulin (SHBG), estradiol, dehydroepiandrosterone (DHEA), cortisol, and thyroid hormones.
Additional tests may assess insulin levels, inflammatory markers, and metabolic health to provide a complete picture of hormonal status. For men over 50, bone density (DEXA) scans are recommended due to hormone-related bone loss risk.
Functional medicine practitioners go beyond lab results, correlating them with a detailed medical history and lifestyle assessment. So as to understand symptoms to ensure a holistic diagnosis, as normal ranges may not reflect optimal health for every individual.
This thorough approach ensures that treatment addresses both symptoms and their underlying drivers, maximizing effectiveness.
The Ideal Candidate for BHRT and TRT
BHRT and TRT are specialized treatments designed to address hormonal imbalances that significantly impact quality of life. These therapies are not suitable for everyone, and candidacy depends on specific symptoms, confirmed hormone deficiencies, medical history, and a commitment to a supervised treatment plan.
Candidates for BHRT and TRT are usually men with clinically diagnosed low testosterone, women experiencing menopause or perimenopause symptoms, and individuals with other hormonal imbalances such as thyroid disorders, adrenal fatigue, or low DHEA levels.
However, individuals with certain conditions, such as untreated prostate cancer, severe heart disease, or uncontrolled sleep apnoea, may not be suitable for TRT due to potential risks. Women with a history of hormone-sensitive cancers (e.g., breast cancer) require careful evaluation before starting BHRT.
Functional medicine broadens the candidacy criteria by focusing on root causes of hormonal imbalances, such as gut health, inflammation, or environmental toxin exposure. This approach benefits individuals who may not have severe deficiencies, but still experience symptoms due to suboptimal hormone function.
That said, anyone experiencing persistent symptoms of hormonal imbalance should consult a healthcare provider specializing in BHRT or TRT for evaluation. Early intervention can prevent long-term complications, such as osteoporosis or cardiovascular disease.
Treatment Options for Hormone Imbalance
Addressing hormonal imbalances requires a multifaceted approach, combining lifestyle interventions, nutritional support, and, when necessary, hormone therapy.
Functional medicine prioritizes lifestyle changes as the first step. A nutrient-dense, anti-inflammatory diet (such as the Mediterranean diet, rich in protein, healthy fats and omega-3 fatty acids) supports hormone production.
Regular exercise, particularly resistance training and high-intensity interval training (HIIT), boosts testosterone levels naturally. Prioritizing 7–9 hours of quality sleep is essential, as is stress management through practices like mindfulness, meditation, or yoga. These practices lower cortisol and support hormonal balance.
Nutritional supplements can further enhance hormone production. Zinc, vitamin D, magnesium, probiotics and gut cleansers are critical for testosterone synthesis. While adaptogenic herbs like ashwagandha, fenugreek, or maca may provide additional support. These natural interventions are often effective for mild deficiencies but may not suffice for more severe cases.
When lifestyle and supplements are insufficient, hormone therapy becomes a valuable option. BHRT addresses a range of hormonal deficiencies using bioidentical hormones administered via creams, gels, patches, injections, or subcutaneous pellets. TRT specifically targets low testosterone, with similar administration methods tailored to the patient’s needs and lifestyle. Both therapies are customized, based on lab results and ongoing monitoring to ensure optimal hormone levels and minimize side effects.
Functional medicine integrates these approaches, combining hormone therapy with lifestyle changes to address root causes like gut health, inflammation, or toxin exposure. This holistic strategy enhances treatment outcomes and promotes long-term wellness.
Benefits of BHRT and TRT
The benefits of BHRT and TRT are transformative. They restore vitality and improve overall health. Physically, these therapies increase energy, muscle mass, and bone density while reducing body fat, enabling individuals to regain strength and stamina.
Sexual health improves significantly, with enhanced libido and better sexual function, addressing common concerns like erectile dysfunction or vaginal dryness. Mentally, patients report improved mood, reduced depression or anxiety, and enhanced cognitive clarity which allows better focus and productivity.
Long-term, BHRT and TRT may reduce the risk of chronic conditions such as osteoporosis, cardiovascular disease, and metabolic disorders. By restoring hormonal balance, these therapies support overall wellness, helping individuals feel more like themselves and improving their quality of life.
Risks and Safety Considerations
While BHRT and TRT offer significant benefits, they are not without risks. TRT may lead to side effects such as increased red blood cell count (polycythemia), acne, hair loss, or sleep apnoea. There is also ongoing debate about potential cardiovascular risks and prostate issues, though evidence remains mixed.
To ensure safety, hormone therapy requires medical supervision, with regular blood tests to monitor prostate-specific antigen (PSA), hematocrit, and lipid profiles. Dosage adjustments based on these results minimize risks and optimize outcomes.
It must also be kept in mind that BHRT and TRT are in essence, a Band-Aid approach for a limited time period. They cannot be depended upon for life. For a sustainable solution, the root causes must be addressed.
Functional medicine mitigates risks by addressing underlying causes alongside hormone therapy. By improving diet, exercise, and stress management, patients can reduce reliance on therapy and enhance its safety and effectiveness.
Getting Started with Hormone Therapy
If you suspect a hormonal imbalance, the first step is to consult a qualified provider specializing in BHRT or TRT. Clinics offer expertise in personalized hormone therapy, while functional medicine practitioners provide a holistic perspective. During your consultation, expect comprehensive lab testing and a thorough evaluation of symptoms and lifestyle. Your provider will discuss administration methods (such as injections, gels, or pellets) and create a tailored plan. Combining therapy with lifestyle changes, such as a nutrient-rich diet and regular exercise, will maximize results and support lasting health. For more info, you can contact our team of experts at Wellfinity.
For John, the 45-year-old struggling with fatigue and low drive, hormone therapy offered a path to reclaim his vitality. Like him, many individuals can benefit from BHRT and TRT to address hormonal imbalances and restore energy, mood, and overall well-being. By combining these therapies with a functional medicine approach which emphasizes lifestyle changes and root-cause solutions, you can achieve lasting health improvements.
If you’re experiencing symptoms of low testosterone or hormonal imbalance, consult a qualified provider to explore personalized treatment options. Take the first step toward feeling like yourself again and embrace a healthier, more vibrant future.



